Editor’s Note: The death of R&B singer D’Angelo earlier this month, following his battle with pancreatic cancer, brought renewed awareness to the disease. This Q&A is part of our occasional Howard University Cancer Awareness Series, which spotlights the scientists, physicians, and partners advancing discovery and equity in cancer research and care. Through pioneering studies, new collaborations, and promotion of early detection, Howard continues its mission to save lives and transform health outcomes in Black and underserved communities.
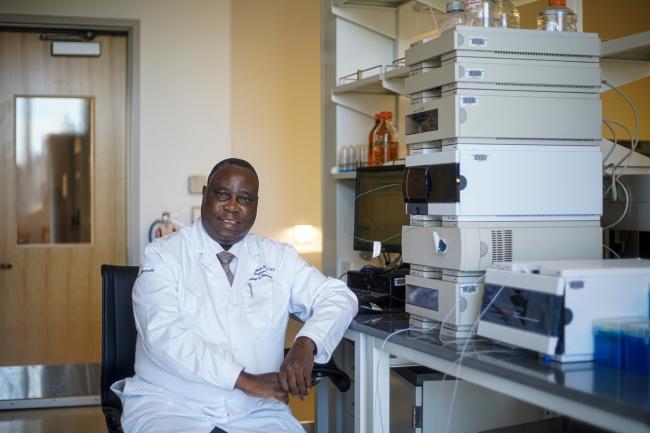
Howard University scientist Emmanuel O. Akala, R.Ph., Ph.D., professor and director of the Center for Drug Research and Development in the College of Pharmacy, is leading a groundbreaking early-stage collaboration with professors Wilfred Ngwa and Kai Ding of the Department of Radiation Oncology and Molecular Radiation Sciences at The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University to develop an innovative treatment for one of the deadliest cancers, pancreatic cancer. In this Q&A, Dr. Akala discusses the science behind the project, how it builds on his pioneering nanotechnology research, and why the work could help reduce longstanding disparities in cancer care.
Q: Dr. Akala, you’ve worked for years at the intersection of biology, chemistry, engineering, pharmacy, and medicine. What drives your current research focus on pancreatic cancer?
A: Pancreatic cancer is one of the most difficult cancers to treat and one of the deadliest. It’s often called a “silent killer” because it’s rarely detected early enough for surgery to be effective. By the time most patients are diagnosed, the cancer has already spread beyond the pancreas. My goal — and our team’s goal — is to develop a more effective, affordable treatment that can truly make a difference in survival rates, especially for Black patients who are often the most affected by disparities in care.
Q: Why makes pancreatic cancer such a challenging cancer to treat?
A: The biggest challenge is that it’s rarely diagnosed early. Unlike breast or prostate cancer, we don’t yet have a reliable screening method to detect pancreatic cancer before it spreads. By the time most patients are diagnosed, the cancer has already metastasized to other organs, which makes surgery ineffective. Only about 20% of patients qualify for surgery, and even then, survival rates remain low. In addition, traditional radiation therapy often damages nearby organs like the liver, kidneys, and small intestine because the pancreas sits deep in the body (visceral tumor that develops in the soft, internal organ of the body). These factors make pancreatic cancer extremely difficult to treat successfully.
Q: Why is pancreatic cancer so deadly?
Pancreas makes enzymes for digesting your food and hormones for regulating blood sugar levels. Exocrine cells of the pancreas make enzymes that help you digest food. About 90% of pancreatic cancer starts as adenocarcinoma tumors in these exocrine cells. Usually, it starts in the cells that surround the pancreatic duct that feeds digestive juices into your small intestine. Endocrine cells make hormones like insulin and glucagon that help regulate your blood sugar. Less than 10% of pancreatic cancers start in these endocrine cells. These cancers are called pancreatic neuroendocrine tumors, and they tend to grow slower than pancreatic adenocarcinoma tumors.
One of the challenges with pancreatic cancer is that the symptoms are often not distinct; the symptoms can be caused by a lot of different conditions that are much more common than pancreatic cancer (diarrhea or indigestion). A person may have early symptoms (digestive symptoms like diarrhea, indigestion, unexplained weight loss, and blood sugar changes) from a pancreatic neuroendocrine tumor than from an adenocarcinoma. A person with adenocarcinoma may develop jaundice (yellowing of the whites of your eyes and skin) early on, before the cancer has grown large or spread outside your pancreas
Q: You’re collaborating with Johns Hopkins University on this project. How did that partnership come about?
A: The project began with a joint grant proposal we submitted in early 2024, and the National Cancer Institute awarded us a five-year grant that fall. Each cancer focus area in the grant has a Howard lead and a Johns Hopkins lead. I’m leading the pancreatic cancer research at Howard, and my colleague Dr. Ngwa is leading the work at Johns Hopkins. It’s a true partnership, with our labs complementing each other’s expertise.
Q: What makes your approach to treatment different from current pancreatic cancer therapies?
A: Our approach brings together flash radiotherapy, a form of radiation delivered in rapid bursts, and smart radiotherapy biomaterials, tiny engineered particles that help target treatment more precisely. By combining these two innovations, we’re developing a new therapy called Proton Enhanced Radio-Immunotherapy with FLASH Effect in Cancer Treatment, or PERFECT for short.
Traditional radiation therapy for pancreatic cancer takes time and often damages nearby organs like the liver or kidneys because the pancreas sits deep among them. With flash radiotherapy, we deliver a large dose of radiation in a millisecond rather than over several minutes or hours. This short burst spares surrounding organs but still delivers a powerful enough dose to kill the cancer cells.
At Howard, my lab develops the small multifunctional nanoparticles — what we call “radio biomaterials” — that enhance the effect of the radiation and make the tumor more visible and responsive.
Q: Can you explain how these nanoparticles work?
A: The nanoparticle has several key components; it is multifunctional. They include a contrast agent to make the tumor more visible, which helps precisely target the radiation. They also include a chemotherapeutic drug to kill the cancer cells and trigger an immune response. Finally, they carry an immunotherapy material that helps the body recognize and attack any remaining cancer cells. Together, this combination turns what we call a “cold tumor” — one that resists immune attack — into a “hot tumor” that the immune system can destroy (makes the tumor immunogenic). Another exciting aspect of our research is that by making the tumor more immunogenic, flash radiotherapy can contribute to stimulating systemic anti-tumor immunity and induce the abscopal effect, where non-irradiated metastases are also targeted and eliminated by the immune system.
Q: Your earlier research used nanotechnology in the search for an HIV cure. How does that experience inform your current cancer work?
A: The science builds on the same foundation. At Howard, I’ve spent years developing nanoparticle systems for drug delivery. In my HIV work, we created nanocarriers that could deliver medication precisely to infected cells and remain effective for long periods. Now, I’m adapting those same engineering principles — targeted, efficient, and sustained delivery — to cancer therapy. Nanotechnology gives us a way to direct powerful treatments to exactly where they’re needed in the body: targeted delivery that precisely delivers the bioactive agents to the biophase (site of action), thereby improving efficacy and avoiding off-target toxicities or side effects.
Q: Pancreatic cancer disproportionately affects African Americans. How could your work help reduce those disparities?
A: Cost and access are major factors in health disparities. Flash radiotherapy is not only more effective, it’s also faster and potentially more affordable. Unlike traditional radiation, where patients must return multiple times, this treatment could be delivered once. That makes it easier for patients who can’t afford to miss work or travel long distances. If we can make this therapy accessible and affordable, we can close the gap in who survives pancreatic cancer.
Q: What stage is the project in now, and what are the next steps?
A: We’re in the early research stage. The Howard team is developing and testing the nanoparticles, and Johns Hopkins is conducting the flash radiotherapy studies. We’re starting with mice, then moving to nonhuman primates (which have genetic similarities to humans) before clinical trials. Our ultimate goal is a treatment that can extend life, improve quality of life, and make pancreatic cancer survivable.
Q: What motivates you personally in this work?
A: Saving lives. Whether it’s HIV, breast cancers (triple negative and HER2-positive breast cancers), or pancreatic cancer, my commitment is to develop technologies that protect and prolong life, especially for people in our community who have been underserved. Science gives us the tools to make that possible.
###
Keep Reading
-
 Homecoming 2025
Homecoming 2025Howard Students Prove They're ‘One of One’ With Win at Inaugural Microsoft AI Policython
Oct 16, 2025 6 minutes -
 News
NewsAuthors and Artists Tell ‘The Story of Us’ at International Black Writers Festival
Oct 7, 2025 7 minutes
Find More Stories Like This
Are You a Member of the Media?
Our public relations team can connect you with faculty experts and answer questions about Howard University news and events.
Submit a Media Inquiry