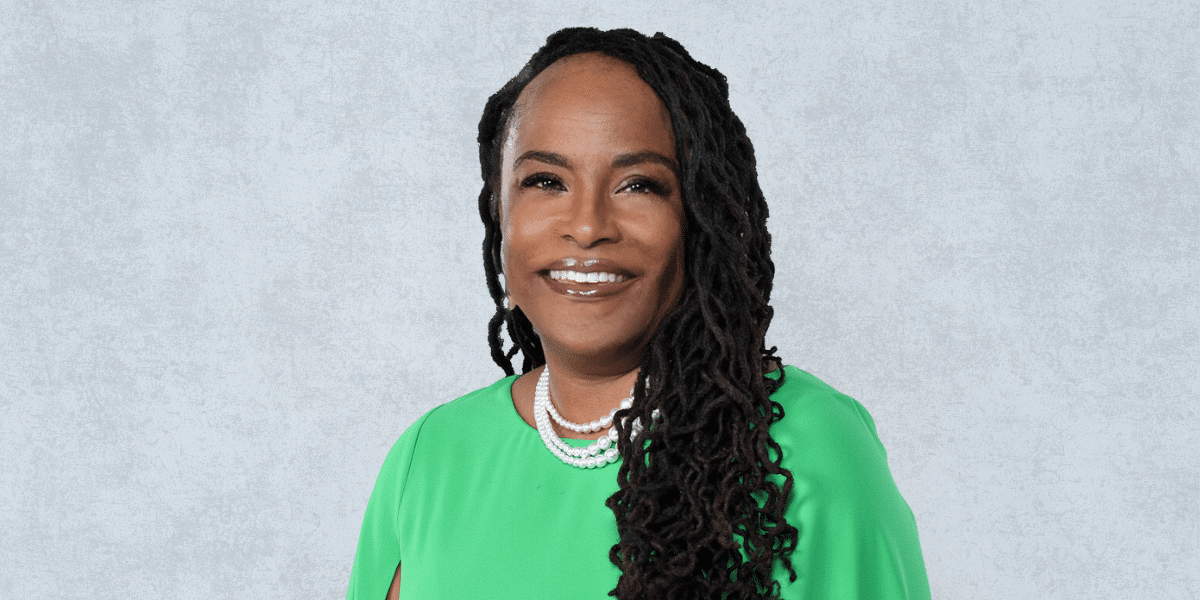
In this special edition of the “Focused on You” series, Coe outlines some symptoms to look out for and related risks, offers advice for screenings and prevention, and shares additional resources to help women be their own advocates.
What is Cancer?
According to ACS, cancer is a “group of diseases characterized by the uncontrolled growth and spread of abnormal cells that can result in death if untreated.” While the causes of most cancers are unknown, the organization points to lifestyle factors and inherited genetic mutations, which can increase risk “either by acting alone or in combination, to initiate and/or promote cancer growth.”
Coe notes that most breast cancers begin in the “milk” producing glands (lobules) or tubes (ducts) of the breasts that connect to the nipple.
Symptoms that a woman can see from breast cancer are related to changes in the glands or ducts of the breast that result from a growth from those areas that can cause a lump or skin changes.
Signs and Symptoms of Breast Cancer
The most common symptoms of breast cancer are a lump or mass in the breast, in addition to other persistent changes to the breast, including swelling skin, redness, skin thickening, and nipple abnormalities (i.e. discharge, flakiness, or pulling of the nipple).
Other Symptoms of Note:
- Dimpling of the breast skin
- Pain in the nipple area
- Change in size or shape of the breast
- Pain in any area of the breast
Remember that breast cancer can still be present when there are no symptoms at all.
Breast Cancer Risks
Being assigned female at birth: Those assigned female at birth are at significantly higher risks of developing breast cancer than those assigned male at birth. However, men can get breast cancer too.
Age: For most patients, regular screenings are recommended beginning at the age of 40. However, breast cancer is more common in African American women under the age of 40, and African American women are also more likely to die from breast cancer regardless of age.
It is important to talk to your doctor about your personal medical history and family history to determine if breast cancer screening should begin for you before age 40.
Personal/Family History: A history of breast cancer in your family increases risks. For example, BRCA1 and BRCA2 genes, the most common genetic mutations, though there are others, increase the risk of developing cancer.
Family members are often reluctant to discuss their personal medical issues, but knowing family conditions in parents, siblings, grandparents, aunts, uncles, and even cousins can make a big difference in determining your risk for breast cancer and whether alternative breast cancer screening recommendations are applicable for you.
If your mother, sister, or daughter is diagnosed with breast cancer, especially if they are under the age of 50, this can indicate a high risk for also developing the cancer. In addition, having two family members from the same side of the family diagnosed at any age, a father or brother with breast cancer, and the presence of any other types of cancer in the family also place you in a higher risk category.
If family members are reluctant to discuss their medical conditions, Coe recommends this talking point: “My doctor has told me that it is important to know family medical history, not only for myself, but for the younger adults and children in our family to know how to better take care of themselves as they get older.”
Knowing your family history is key to determining if you need more than annual mammograms for breast cancer, starting at age 40. Genetic testing may be recommended based on family history.
Check with your city, county, and state health departments, as many departments across the country have low cost or free mammogram programs. There are also related resources specifically for the Black community, including The Black Genes Matter Movement, which provides education and resources to help people better “understand their genetic makeup and make informed decisions about their health.”
Lifestyle Risks: It’s not surprising to learn that things like higher alcohol usage, a diet that is high in red meat and processed foods but low in fruits and vegetables, and a lack of exercise and being overweight impact overall health and also increase risks related to developing cancers, including breast cancer. Unlike risks you can’t control (age, gender at birth, family history, inherited genes), these risks can be minimized with lifestyle changes.
Smoking is a huge risk for developing most cancer types. For someone who smokes, quitting goes a long way in decreasing overall cancer risk.
Other Factors: Starting your period early or experiencing menopause later than “normal” could be linked to developing breast cancer, as could things like having dense breast tissue, being diagnosed previously with a benign breast condition, or having received radiation to the chest. While these are not all red flags, the normalcy of them further emphasizes why screenings are so important.
It is important to discuss the factors in your medical care that may increase your risk for breast cancer and work on changing the risks that you can do something about.
Screenings and Prevention
Again, women at average risk for breast cancer should start receiving annual breast cancer screenings at the age of 40. However, if you are at a higher risk of developing breast cancer, especially those with a known family history, screenings may need to happen earlier, in addition to possibly genetic testing, seeing a genetic counselor, and getting more frequent mammograms and/or MRI’s of the breast.
Talk to your doctor about whether seeing a genetic counselor or getting genetic testing is appropriate for you. Depending on family history and genetic testing results, breast cancer screening may need to start as early as age 25-30 with clinical breast exams (a breast exam done by a health care professional), mammograms, and/or breast MRI’s.
While not a substitute for annual mammograms, regularly performing “self-exams” are one way to identify any changes in your breasts that may lead to early detection. BreastCancer.Org offers five steps for checking your breasts at home, including conducting the examination in the mirror with hands on hips, raising arms above the head, looking for signs of swelling, feeling for lumps while laying down, and feeling again while standing or sitting.
Coe recommends having a breast exam reminder card in the shower or setting a monthly alarm on your phone for a reminder to do self-breast exams. Doing a regular self-breast exam allows you to get to know what your breast tissue feels like and makes you more likely to notice a change in your breasts. Self-breast exams should be done one week after the period of menstruation has ended, as breast tissue can be lumpier or tender during menstruation. According to the doctor, while mammograms and breast MRI’s drive most breast cancer screening, the detection of a breast mass that one can feel is defined as a symptom that requires immediate evaluation. Breast masses are often first noted by the patient themselves (patient self-detection) or during a clinical breast exam.